
Incontinence – the involuntary loss of bladder or bowel control – is a condition often shrouded in silence and stigma. Yet, it affects millions worldwide, cutting across all demographics and significantly impacting quality of life. Far from being a minor inconvenience, the comprehensive impact of incontinence extends to physical, emotional, social, and economic spheres. This blog post aims to shed light on this pervasive condition, drawing on medical literature to highlight its prevalence, severity, and multifaceted effects.
Understanding the Scope: Prevalence and Demographics
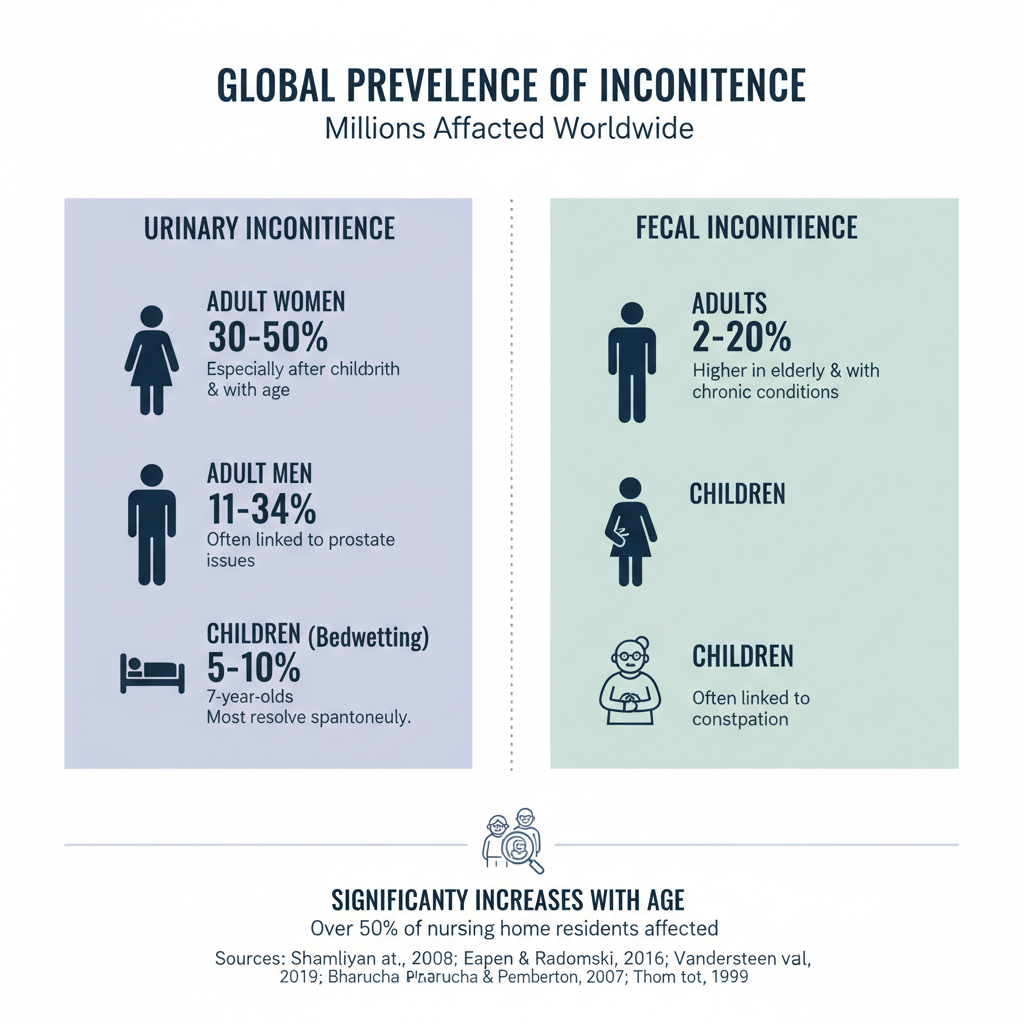
Incontinence is not a rare condition; it’s a widespread public health concern. Its prevalence varies significantly based on age, sex, and the type of incontinence.
Urinary Incontinence (UI):
- Women: UI is considerably more common in women than men, largely due to factors like pregnancy, childbirth, and menopause. Studies suggest that up to 30-50% of adult women experience some form of UI (Shamliyan et al., 2008). This number often increases with age.
- Men: While less common, UI in men is often associated with prostate issues, surgery (e.g., prostatectomy), or neurological conditions. Estimates suggest 11-34% of men experience UI (Eapen & Radomski, 2016).
- Children: Childhood UI, particularly nocturnal enuresis (bedwetting), is common, affecting about 5-10% of 7-year-olds, with most resolving spontaneously (Vandersteen et al., 2019).
- Elderly: Age is a significant risk factor, with prevalence rates soaring in older populations. Over 50% of nursing home residents experience UI (Thom et al., 2999).
Fecal Incontinence (FI):
- FI is generally less common than UI but still affects a substantial portion of the population. Prevalence estimates range from 2% to 20% in the general adult population, with higher rates in older adults and those with underlying medical conditions (Bharucha & Pemberton, 2007).
- Similar to UI, FI can also affect children, often linked to chronic constipation.
The following image illustrates the general prevalence of incontinence.
Beyond the Bladder: The Physical and Mental Health Toll
The impact of incontinence extends far beyond the direct experience of leakage. It significantly affects both physical and mental well-being.
Physical Health Consequences:
- Skin Irritation and Infections: Constant exposure to urine or feces can lead to skin breakdown, rashes, pressure ulcers, and recurrent urinary tract infections (UTIs) (Nazarko, 2011).
- Sleep Disturbances: Frequent nocturnal urination (nocturia) due to UI can disrupt sleep patterns, leading to fatigue, irritability, and decreased cognitive function (Breyer et al., 2017).
- Falls: Rushing to the toilet, especially at night, can increase the risk of falls, particularly in older adults, leading to serious injuries (Huang et al., 2018).
- Activity Restriction: Fear of leakage can lead individuals to limit physical activity, exacerbating other health issues like obesity and cardiovascular disease.
Mental and Emotional Health Consequences:
- Embarrassment and Shame: The stigma associated with incontinence often leads to feelings of embarrassment, shame, and isolation.
- Anxiety and Depression: The constant worry about accidents, the disruption to daily life, and the social limitations can significantly contribute to anxiety and depression. Studies show a higher prevalence of depression among individuals with UI (Coyne et al., 2004).
- Loss of Self-Esteem: Incontinence can erode self-esteem and body image, impacting personal relationships and overall confidence.
- Social Isolation: Many individuals with incontinence withdraw from social activities, travel, and even work to avoid potential embarrassing situations, leading to social isolation.
Here’s an illustration of the multifaceted impact on a person’s life:
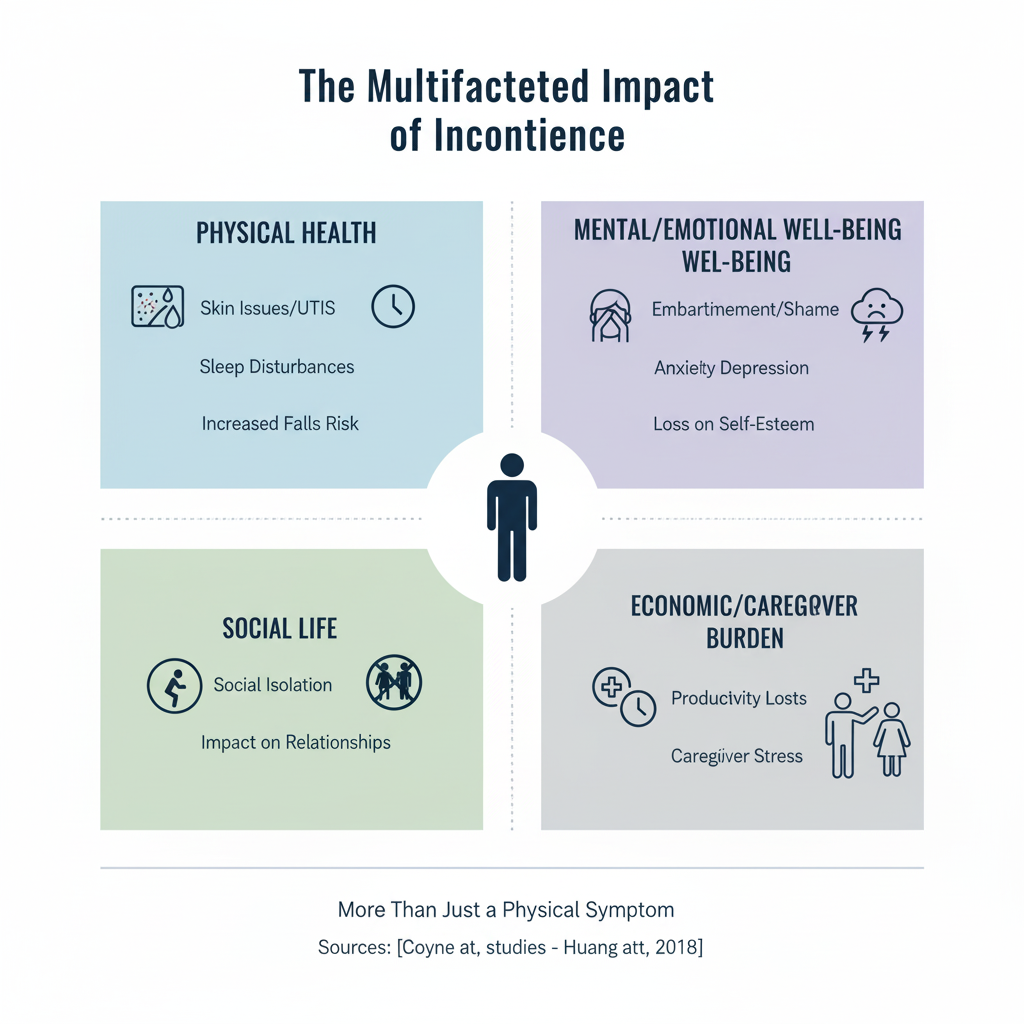
The Ripple Effect: Social and Economic Burdens
The impact of incontinence extends beyond the individual, affecting families, caregivers, and healthcare systems.
Social Impact:
- Relationship Strain: Incontinence can strain intimate relationships, impacting sexual health and intimacy due to embarrassment or fear of leakage.
- Caregiver Burden: For those caring for individuals with incontinence (e.g., elderly parents, children with special needs), the demands of managing the condition can be physically and emotionally exhausting, leading to caregiver stress and burnout (Schulz & Martire, 2004).
Economic Impact:
- Direct Costs: These include the expenses for absorbent products (pads, diapers), medications, doctor visits, diagnostic tests, and surgeries. These costs can be substantial, especially for chronic incontinence.
- Indirect Costs: These are harder to quantify but include lost productivity at work due to absenteeism or reduced efficiency, early retirement, and the costs associated with managing related health complications (e.g., UTIs, falls).
- Healthcare System Burden: Incontinence contributes significantly to healthcare expenditures, including hospitalizations, emergency room visits, and long-term care placements.
Breaking the Silence: Seeking Help and Management
Despite its widespread impact, incontinence remains underreported and undertreated. Many individuals suffer in silence due to embarrassment or the misconception that it’s a normal part of aging. However, it’s crucial to remember that incontinence is a treatable and manageable condition.
Key Steps to Management:
- Consult a Healthcare Professional: The first and most important step is to talk to a doctor. They can diagnose the type and cause of incontinence and recommend appropriate treatment options.
- Lifestyle Modifications: These can include dietary changes, fluid management, weight loss, and avoiding bladder irritants.
- Pelvic Floor Muscle Training (Kegel Exercises): Strengthening the pelvic floor muscles can significantly improve UI, especially stress incontinence.
- Medications: Various medications are available to help manage overactive bladder symptoms.
- Behavioral Therapies: Bladder training and timed voiding can help regain bladder control.
- Medical Devices and Procedures: Options like pessaries for women, nerve stimulation, or even surgery may be considered for more severe cases.
- Absorbent Products: While not a cure, high-quality absorbent products can provide comfort and confidence in managing leaks.
- Support Groups: Connecting with others who experience incontinence can provide emotional support and practical advice.
Conclusion
Incontinence is a complex and often debilitating condition with far-reaching consequences for individuals, families, and society. By understanding its prevalence, diverse impacts, and the available management strategies, we can work towards breaking the stigma, encouraging open dialogue, and ensuring that those affected receive the support and treatment they need to improve their quality of life. Remember, you are not alone, and help is available.
References:
- Bharucha, A. E., & Pemberton, J. H. (2007). Fecal incontinence. Gastroenterology, 132(6), 2050-2065.
- Breyer, B. N., Shindel, A. W., & Husain, A. (2017). The association of nocturia with sleep disturbance and daytime somnolence in men. BJU International, 119(3), 481-487.
- Coyne, K. S., Zhou, Z., Bhattacharyya, S. K., & Brubaker, L. (2004). The burden of overactive bladder on health-related quality of life and work productivity in five European countries. BJU International, 93(7), 1022-1029.
- Eapen, R. S., & Radomski, S. B. (2016). Etiology and pathophysiology of male urinary incontinence. Translational Andrology and Urology, 5(1), 2-12.
- Huang, A. J., Subak, L. L., & Thom, D. H. (2018). Urinary incontinence and falls in older women. Journal of the American Geriatrics Society, 66(6), 1146-1153.
- Nazarko, L. (2011). Protecting skin from incontinence-associated dermatitis. British Journal of Community Nursing, 16(3), 112-117.
- Schulz, R., & Martire, L. M. (2004). Family caregiving of persons with dementia: prevalence, health effects, and support strategies. The American Journal of Geriatric Psychiatry, 12(3), 240-249.
- Shamliyan, T. A., Kane, R. L., & Wyman, J. F. (2008). Systematic review: randomized, controlled trials of nonsurgical treatments for urinary incontinence in women. Annals of Internal Medicine, 148(6), 459-473.
- Thom, D. H., Hanley, J., & Wood, R. (1999). Prevalence and correlates of incontinence in a community sample of women 60 years of age and older. The Journal of the American Geriatrics Society, 47(6), 675-682.
- Vandersteen, D. R., Routh, J. C., & Wiener, J. S. (2019). The current epidemiology and natural history of enuresis. Current Urology Reports, 20(4), 16.
